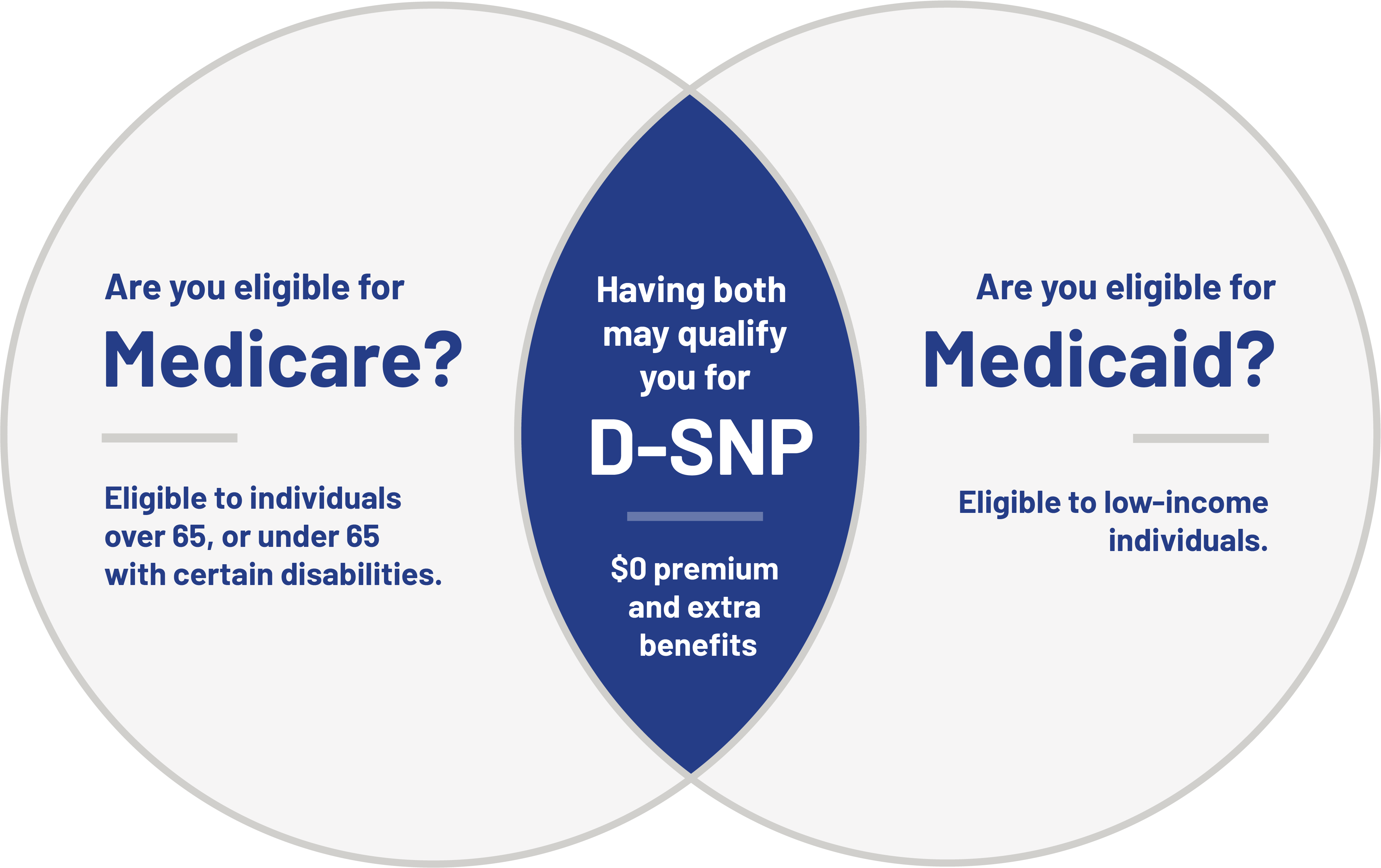
Do you have Medicaid (OHP) and Medicare?
You may qualify for a $0 Providence Medicare Dual Plus (HMO D-SNP) plan with up to $800 for food and produce, $0 prescriptions, a $900 allowance for dental and more.
503-574-6836 (TTY: 711)
Get more benefits on a $0 Providence Medicare
D-SNP plan
A Dual Special Needs Plan (D-SNP) coordinates your Medicare, Medicaid (also known as Oregon Health Plan), and Part D prescription benefits to give you a more focused care plan. The $0 Providence Medicare D-SNP plan covers everything under Original Medicare plus many extra benefits and services, including:
Learn more about the benefits of a D-SNP plan
See if you qualify
The following are requirements that may qualify you for a Providence Medicare D-SNP plan:
- Dual eligibility - Qualify for both Medicare and Medicaid - OHP.
- Reside in the area of service - the Providence Medicare D-SNP plan is currently available in Oregon in Multnomah, Washington and Clackamas counties.
- Residency - U.S. citizen or have legal permanent residency.
When can I enroll?
If you already have both Medicare and Medicaid (OHP), or you already have a D-SNP,
call us to see when you can switch plans.
503-574-6836 (TTY: 711) 8 a.m. to 5 p.m. Monday through Friday (Pacific Time)
Explore our D-SNP benefits in detail
Download the Providence D-SNP benefit highlights guide to learn about advantages and services available to you. Just fill out the form to download.
Need more information about Providence D-SNP?
Download the Enrollment Guide for essential information, enrollment options available to you, and what to do next. Just fill out the form to download.
Legal
Disclaimers & things to know
*This benefit is part of a special supplemental program for the chronically ill. Members with diabetes mellitus, chronic and disabling mental health conditions, cardiovascular disorders, chronic lung disorders, neurologic disorders, and other eligible conditions not listed may qualify to receive this benefit. Eligibility for this benefit cannot be guaranteed based solely on your condition. All applicable eligibility requirements must be met before the benefit is provided.
For accommodations of persons with special needs at meetings call 503-574-7756 or 888-804-5148 (TTY: 711).
Providence Health Assurance is an HMO, HMO-POS and HMO SNP with Medicare and Oregon Health Plan contracts. Enrollment in Providence Health Assurance depends on contract renewal.
For a complete list of available plans please contact 1-800-MEDICARE (TTY users should call 1-877-486-2048), 24 hours a day/7 days a week or consult www.medicare.gov.
We're here for you. If you need assistance or have questions please reach out to our customer service team at 503-574-8000 or 1-800-603-2340 TTY: 711 8 a.m. to 8 p.m. (Pacific Time) 7 days a week, October 1st through March 31st and Monday - Friday, April 1st through September 30th.
To file a complaint about our marketing, you may call us at 1-800-603-2340 (TTY: 711) 8 a.m. to 8 p.m. (Pacific Time) 7 days a week, October 1st through March 31st and Monday - Friday, April 1st through September 30th, by calling Medicare at 1-800-MEDICARE, 24/7, or by submitting an online form at www.medicare.gov. If you experienced issues with agents or brokers, please include their name in the complaint if possible.
Webpage is current as of: 10/01/2025




